About Lupus nephritis1-3
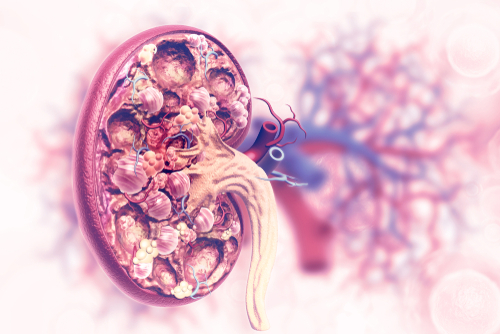
Lupus nephritis is considered an Orphan disease, with around 80,000 – 100,000 patients in U.S, and 1 million worldwide. It is one of the most serious manifestations of systemic lupus erythematosus (SLE), occurring in 50 – 60% of patients, typically within 5 years of diagnosis. Nephritis is evident in most SLE patients’ biopsies, including those with no symptoms of kidney disease.
As with other kidney diseases, the symptoms are related to high blood pressure, protein spillage into the urine (proteinuria), and kidney failure. Symptoms include edema, headaches, dizziness, nausea, and vomiting. It is the nephritis symptoms that often drive patients to seek medical care, leading to the diagnosis of SLE.
Nephrotic syndrome may lead to edema, ascites, and hyperlipidemia, adding to the risk of coronary artery disease and the potential for thrombosis (formation of clots in blood vessels). Findings from one study indicate that patients with lupus nephritis, particularly early-onset lupus nephritis, are at increased risk for morbidity from ischemic heart disease.
The goal of therapy is to prevent progressive loss of kidney function, and ideally to normalize function. Therapy differs depending on the pathologic lesion, as it is important to treat extrarenal manifestations and other variables that may affect the kidneys. All patients receive background therapy of hydroxychloroquine, unless contraindicated. There are no renal-specific drugs approved for lupus nephritis. Treatment of kidney manifestations of SLE is similar to that of other kidney diseases, with ACE inhibitors and ARBs used to control hypertension, and corticosteroids as the mainstay for treating proteinuria, followed by immunosuppressive agents in non-responding patients. Patients with end-stage renal disease are unlikely to respond to aggressive therapy and require dialysis or kidney transplant.
Morbidity associated with lupus nephritis is related to the renal disease itself, as well as to treatment-related complications and comorbidities, including cardiovascular disease and thrombotic events. Progressive renal failure leads to anemia, uremia, and electrolyte and acid-based abnormalities. Hypertension may lead to an increased risk of coronary artery disease and stroke . Nephrotic syndrome may lead to edema, ascites, and hyperlipidemia, adding to the risk of coronary artery disease and the potential for thrombosis. The findings from one study indicate that patients with lupus nephritis, particularly early-onset lupus nephritis, are at increased risk for morbidity from ischemic heart disease.
There is a significant unmet need for effective lupus nephritis-specific treatments that can delay disease progression, prevent end-stage renal disease, and improve patients’ quality of life.
References
- CDC
- Lupus Fact Sheet
- Brent LH et al: Lupus Nephritis. Medscape, updated 3/4/19